
Visits from New York State Governor Kathy Hochul with SUNY Upstate President Mantosh Dewan, MD, and Upstate University Hospital CEO Robert Corona, DO, helped to build understanding of the infrastructure needs of Upstate University Hospital. To serve the population being seen at Upstate, key elements of the annex are an expanded Emergency Department providing Upstate with between 55 and 75 bays, compared to the current 35. Also, planned: a new burn unit with between six and eight ICU beds and the addition of between two and four new operating room.
When an organization consistently focuses on innovation over a period, growth and expansion are often the result. This pattern certainly has been the case with Upstate University Hospital, which includes its main campus in Syracuse and many adjacent healthcare facilities located throughout Central New York.
As Central New York’s only academic medical center, as well as the region’s largest employer, Upstate has been exploring and utilizing new and innovative healthcare initiatives for years under the leadership of Robert Corona, DO, CPE, MBA, FCAP, FASCP, who has served as CEO of the hospital since 2018. A new throughput center, a new pathology institute presently under construction, cutting-edge drone technology, new clinical offerings and innovative, eco friendly buildings are just a few of the ways Upstate has been on the forefront of advancements in healthcare. Stemming from innovations in these varied aspects of healthcare, Upstate is now experiencing a period of immense growth.
Alongside these offerings, the big news announced in May 2025 was that Governor Kathy Hochul and the New York State Legislature had allocated $450 million in the state budget for Upstate to build a new and expanded emergency department, a more modern burn unit, and some additional operating room capacity at its downtown Syracuse campus. This support of a hospital “annex” represents the largest capital funding allocation in Upstate’s history.
“There’s just a ton of growth happening,” said Dr. Corona. “It’s exciting. And while it’s a challenge to stay on top of all the building and expansion we’re doing, overall, if you ask me how I feel, I’m very excited about it all.”
Expanding to Better Serve Patients in CNY
Dr. Corona described that prior to the capital funding announcement, Governor Hochul visited Upstate’s emergency department and recognized the need for expanded services to help meet the community’s needs. He also emphasized the immense support the Upstate team received from the state legislators who “all went to bat for us.” “The governor came and visited our emergency department a couple of times. She was very gracious. And when she saw the status of the physical plant and the contrast of that with the exceptional people who work there, she felt the people of Central New York need a better emergency department, especially when this is the go-to referral center. And she surprised us with the $450 million, which we’re so grateful for,” Dr. Corona said.
Elaborating on the demand for greater capacity to serve patients in the community, Dr. Corona stated that the Upstate healthcare system needs more capacity including operating rooms, and a bigger emergency department to support its level one trauma center. Additionally, an upgraded burn unit is needed because Upstate is the only burn unit between Rochester and Westchester County.


LOW-DOSE RADIATION THERAPY
Upstate Medical University now offers low-dose radiotherapy to treat osteoarthritis. This provides safe, effective, and non-invasive treatment for inflammatory and degenerative conditions of the tendons, joints, and other soft tissues of the body. It can significantly improve pain and stiffness, helping avoid the need for surgery. Anna Shaprio, MD, of Upstate’s Department of Radiation Oncology leads this program and is accepting patients for treatment
“We have a responsibility to our community to grow our capacity,” Dr. Corona stated.
Speaking about the timeline of the hospital annex, Dr. Corona said an aggressive timeline would be about five years. Selection of a design team is already underway, and the team is hoping to have a design company selected by the end of 2025. Following the selection will be collaboration with healthcare providers who work in the affected environments, analysis of demolition needs, and finally, construction.
Reflecting on the magnitude of this growth at Upstate, Dr. Corona said, “I think this has got to be one of the highlights of my career.”
Looking at Growth Through Various Lenses
Not to be overshadowed by the historic capital funding for the main hospital annex is the surge in growth happening within Upstate’s new and existing locations throughout the wider rural Central New York region. The theme of “meeting people where they are” has consistently driven the strategic vision of growth carried out by Dr. Corona and the C-suite team at Upstate. To further develop hospital services and facilities that meet patients’ needs closer to where they live, Dr. Corona explained how he views growth through several lenses, including both the specific population and the geographic region being served.
 “Those are the two main things we look at when we consider strategically where we’re going to grow,” he said.
“Those are the two main things we look at when we consider strategically where we’re going to grow,” he said.
When looking at growth through the lens of the population, Dr. Corona explained that the group of people that’s presently the most prevalent is the mature population, who are living longer with chronic diseases such as heart disease, cancer, cerebrovascular diseases, diabetes and neurologic diseases such as Alzheimer’s. Looking to the future, Dr. Corona anticipates a younger demographic of patients that will create the need for a different set of healthcare needs.

REGION’S ONLY MULTI-DISCIPLINARY MELANOMA PROGRAM
The Melanoma and Advanced Skin Cancer Program at the Upstate Cancer Center is the region’s only multi-disciplinary team and treats melanoma, advanced basal and squamous cell cancers and rare skin cancers such as Merkel cell carcinoma and others. From left: Daniel Thomas, MD, Amar Suryadevara, MD, Scott Albert, MD and Jade Homsi, MD.
“If you look at the population we anticipate coming to the region, that’s going to be families that are going to be working at places like Micron and some of the other new companies that are coming in the area,” Dr. Corona said. “In Rome, Chobani Yogurt is building a large plant and so we anticipate that will also create high demand for our primary care services, family medicine, OB/GYN and pediatrics. We plan to expand the services we offer east of Syracuse, leveraging our success in Verona.”
Looking through the lens of geographic need, and helping patients access healthcare closer to where they live, Upstate is expanding its cancer care locations at the compass points North, West, and East, with expanded hours and physical locations. The new pathology institute near the existing Bone and Joint Center in East Syracuse should be completed in about 15 months.
“Many patients don’t want to come to downtown Syracuse unless necessary. If they live in rural communities, they want to stay for services in their communities,” said Dr. Corona.
 To provide local care for the anticipated new arrivals near the Micron site in the North and needs in the West, additional expansions have been planned or were already completed at the Liverpool/ Clay Carling Road location, including pediatric care this year, and Upstate’s eighth location for physical medicine and rehabilitation that was finalized last year. Upstate also provides more than a dozen services in the Camillus area to help meet patient needs.
To provide local care for the anticipated new arrivals near the Micron site in the North and needs in the West, additional expansions have been planned or were already completed at the Liverpool/ Clay Carling Road location, including pediatric care this year, and Upstate’s eighth location for physical medicine and rehabilitation that was finalized last year. Upstate also provides more than a dozen services in the Camillus area to help meet patient needs.
The Behind-the-Scenes Operational Side of Growth
Carefully coordinating and directing the operations of the many expansion projects at Upstate is Marylin Galimi, MS, CHOP, Upstate’s Chief Operating Officer. With a background in electrical engineering, Galimi came to Upstate in 2016 and now oversees the development and planning of construction projects in addition to support areas like physical planning, environmental services and supply chain, as well as ancillary services such as radiology, pathology and pharmacy.
Looking back on her almost ten years with Upstate so far, Galimi said, “It’s been a lot of fun to be honest. Just to see and be a part of the growth and the transformation at Upstate has been amazing. I think the community has embraced all the work that we’ve been putting into the community.”
While it’s difficult to give a specific number as projects are started and completed regularly, she estimates there are between 80 to 120 active projects that the Upstate team is working on at any given time. Galimi highlighted the teams involved in the various aspects of these expansion projects.
“We have in-house architects, construction managers, engineers, and the physical planners who work on critical maintenance,” Galimi said. “We even have our own mini construction team that works on construction and renovations.”
The operations leadership team has a unique name: COLT (Clinical Operations Leadership Team), which meets weekly to work through operational initiatives and to keep growth moving forward in-line with Upstate’s mission and vision.
“The group is unique and it’s effective. It really helps us stay on track,” said Galimi, adding that participants include other members of the C-suite: CMO Amy Tucker, MD; CNO Scott Jessie; CAO Nancy Daoust; CIO Mark Zeman and Laurie Nicoletti from the CEO’s office.
“The composition of the group is what makes it successful,” she added. “We elevate items to the CEO for final approval and, as needed, review financial impacts with the CFO or staffing with the CHRO.”
When planning new projects, such as the recently completed Interventional Radiology Suite, Galimi explained the most important considerations for her and the team are the people who will be working within the buildings – both now and in the future – so that care can be provided in the best way possible for patients.

MINIMALLY INVASIVE LUNG BIOPSIES
Manju Paul, MD, and Mansur Javaid, MD, are in the suite where they offer minimally invasive robotic-assisted lung biopsy which enables doctors to detect lung cancers much earlier than other methods. Upstate is the only hospital in the region to offer this procedure.
“It’s like we’re building the house, and the people who are going to be inside the house —those who will be providing the services and the patients who will receive care— are the most important part of the plan,” she said. “So, we work on how we’re going to create an environment that will attract new recruits to the area and make it more efficient for the people working inside the space to provide the services they’re skilled to do, and ultimately make it the best experience for the patient.”
Patient-Centered Expansion and Collaboration
No matter where the new projects are taking place, whether it’s the hospital annex in downtown Syracuse or brandnew healthcare centers in rural areas, Galimi emphasized how each area of growth that Upstate pursues is aimed at meeting patients where they are.
“We’re always looking at multiple growth paths in parallel,” she said. “We’re looking at how we get services to the patients where they are. We’re not just doing one thing in the Syracuse city area – we’re growing for the entire Central New York region.”
For Dr. Corona, an exciting aspect of Upstate’s mission to expand into areas that will help meet the needs of patients throughout the community is the opportunity to collaborate with other healthcare organizations.
“I see a tremendous opportunity for collaboration among the hospitals in the region to work as a system, for needs like load balancing and keeping patients in their own communities,” he said. “We support that. And the growth is big enough that everybody could grow. Competition can be healthy and move care forward but there is a lot of collaboration and that’s a really nice thing to see.”
As Galimi pointed out as well, such patient-centered collaboration benefits everyone. “I think what I value most about Upstate is that it’s looking at total health and wellness of the entire community,” she said.


 I will not debate the politics behind the recent health care cuts, but I will share my concerns about their impacts.
I will not debate the politics behind the recent health care cuts, but I will share my concerns about their impacts.
 From breast cancer surgery, hernia repairs and laparoscopic surgery, to endocrine surgery, ulcer care, bariatric surgery and more, the Crouse Medical Practice General Surgery team offers a wide array of surgical procedures to help patients return to health and continue enjoying their lives. The team of 12 physicians brings a vast depth of knowledge and experience that combine to create a supportive practice that consistently focuses on patient-centered care. This patient-focused philosophy is built upon collaboration with the team, including primary care providers, as Clinton Ingersol, MD, Hillary McMullin, MD, Benjamin Sadowitz, MD, FACS and Angelina Schwartz, MD each explained in their own words.
From breast cancer surgery, hernia repairs and laparoscopic surgery, to endocrine surgery, ulcer care, bariatric surgery and more, the Crouse Medical Practice General Surgery team offers a wide array of surgical procedures to help patients return to health and continue enjoying their lives. The team of 12 physicians brings a vast depth of knowledge and experience that combine to create a supportive practice that consistently focuses on patient-centered care. This patient-focused philosophy is built upon collaboration with the team, including primary care providers, as Clinton Ingersol, MD, Hillary McMullin, MD, Benjamin Sadowitz, MD, FACS and Angelina Schwartz, MD each explained in their own words.
 Similarly, for Dr. Schwartz, her approach to patient care is focused on open communication and reaching decisions together as a team.
Similarly, for Dr. Schwartz, her approach to patient care is focused on open communication and reaching decisions together as a team. Open lines of communication and support apply not only to patient care, but also to how the team works together to provide optimal healthcare for patients, as Dr. Schwartz emphasized.
Open lines of communication and support apply not only to patient care, but also to how the team works together to provide optimal healthcare for patients, as Dr. Schwartz emphasized. Dr. Ingersol echoed these ideas, highlighting the streamlined communication process within the Crouse healthcare network specifically. “It’s great for patients when everyone is on the same page and communicating in a multidisciplinary fashion. Especially within the Crouse network, it’s so easy to communicate with our primary care colleagues. We can send direct messages to each other to coordinate patient care and ask questions. Our office staff does a great job of coordinating referrals from primary care offices, making sure that patients are seen according to urgency, and making sure things are followed up on and communicated properly,” he explained.
Dr. Ingersol echoed these ideas, highlighting the streamlined communication process within the Crouse healthcare network specifically. “It’s great for patients when everyone is on the same page and communicating in a multidisciplinary fashion. Especially within the Crouse network, it’s so easy to communicate with our primary care colleagues. We can send direct messages to each other to coordinate patient care and ask questions. Our office staff does a great job of coordinating referrals from primary care offices, making sure that patients are seen according to urgency, and making sure things are followed up on and communicated properly,” he explained. “Our senior partner, Dr. Schu, has been great to work with, has been a very willing mentor, and we frequently do cases together. There’s been a lot of exchange of ideas and techniques because I bring in certain expertise, knowledge and biases and he has this wealth of experience and way of doing things. Having all of that at our disposal to decide what is in the best interest of patients is really valuable,” Dr. Ingersol explained. “Any time I have a case that I anticipate being difficult or may run into something I wasn’t anticipating preoperatively, there’s always someone who’s more than willing to come in and take a look or join me if needed. That’s one of the advantages of a big group that has so much experience.”
“Our senior partner, Dr. Schu, has been great to work with, has been a very willing mentor, and we frequently do cases together. There’s been a lot of exchange of ideas and techniques because I bring in certain expertise, knowledge and biases and he has this wealth of experience and way of doing things. Having all of that at our disposal to decide what is in the best interest of patients is really valuable,” Dr. Ingersol explained. “Any time I have a case that I anticipate being difficult or may run into something I wasn’t anticipating preoperatively, there’s always someone who’s more than willing to come in and take a look or join me if needed. That’s one of the advantages of a big group that has so much experience.”
 “In thyroid care, one thing that we’re starting to look into is a new technology called RFA, or radiofrequency ablation,” Dr. Ingersol said. “We’re not in an active phase yet, but it’s something that’s in the near future across the country and becoming a popular modality of treating thyroid nodules.”
“In thyroid care, one thing that we’re starting to look into is a new technology called RFA, or radiofrequency ablation,” Dr. Ingersol said. “We’re not in an active phase yet, but it’s something that’s in the near future across the country and becoming a popular modality of treating thyroid nodules.”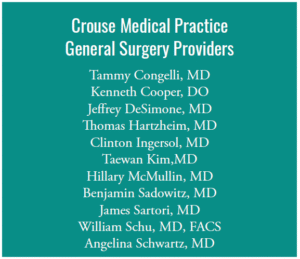 With an administration that invests in cutting edge technologies, and a team of forward-looking surgeons always interested in the latest up-and-coming treatments for patients, it seems the Crouse Medical Practice General Surgery team is well-prepared for the evolving needs of patients and will continue to thrive.
With an administration that invests in cutting edge technologies, and a team of forward-looking surgeons always interested in the latest up-and-coming treatments for patients, it seems the Crouse Medical Practice General Surgery team is well-prepared for the evolving needs of patients and will continue to thrive. “The future is very bright for Crouse in terms of overall surgery, with many great surgeons and a lot of advanced technology. The administration has made it a priority to make sure we stay technologically ahead of the game, so that’s a big piece of it,” said Dr. Sadowitz. “Crouse has always had the right mindset of ‘patients come first’ from the top down. The hospital always aims to keep very talented people in the hospital doing cases, so that not only are the patients highly satisfied, but the surgeons are, too. It’s a unique mix you really don’t find in many places, and it’s a hard balance to maintain, but Crouse has always excelled at doing just that, and as long as we keep that focus, I think it will continue into the future.”
“The future is very bright for Crouse in terms of overall surgery, with many great surgeons and a lot of advanced technology. The administration has made it a priority to make sure we stay technologically ahead of the game, so that’s a big piece of it,” said Dr. Sadowitz. “Crouse has always had the right mindset of ‘patients come first’ from the top down. The hospital always aims to keep very talented people in the hospital doing cases, so that not only are the patients highly satisfied, but the surgeons are, too. It’s a unique mix you really don’t find in many places, and it’s a hard balance to maintain, but Crouse has always excelled at doing just that, and as long as we keep that focus, I think it will continue into the future.” When I asked Andrea what guidance she gives clinicians whose patients are aging and asking questions about the future, she emphasized the importance of early planning. Her advice: choose the best housing option early so you can age in place.
When I asked Andrea what guidance she gives clinicians whose patients are aging and asking questions about the future, she emphasized the importance of early planning. Her advice: choose the best housing option early so you can age in place. Technology plays a major role in the healthcare sector’s ability to store and handle private patient data. This has improved the efficiency of healthcare delivery, but it has also increased the susceptibility of healthcare providers to cyberattacks. The healthcare industry has witnessed a rise in cyber threats, including ransomware attacks, phishing scams, and data breaches. As a result, medical professionals need to take precautions against online threats to both themselves and their patients. A comprehensive Cyber insurance policy is one way to accomplish this.
Technology plays a major role in the healthcare sector’s ability to store and handle private patient data. This has improved the efficiency of healthcare delivery, but it has also increased the susceptibility of healthcare providers to cyberattacks. The healthcare industry has witnessed a rise in cyber threats, including ransomware attacks, phishing scams, and data breaches. As a result, medical professionals need to take precautions against online threats to both themselves and their patients. A comprehensive Cyber insurance policy is one way to accomplish this.

 Almost two years ago, New York enacted PHL Article 45 A, which took effect on August 31, 2023. One of the intents behind this law was flagging large business consolidation in the healthcare field, potentially allowing New York’s Department of Health to regulate the increased transaction prices, reduced competition, or narrowed access to healthcare for residents of the state. Please see our previous article formore information on PHL 45-A here. Importantly, New York’s statute includes Managed Services Organizations (“MSOs”), even though they do not provide healthcare services themselves, as part of any healthcarerelated transaction subject to review.
Almost two years ago, New York enacted PHL Article 45 A, which took effect on August 31, 2023. One of the intents behind this law was flagging large business consolidation in the healthcare field, potentially allowing New York’s Department of Health to regulate the increased transaction prices, reduced competition, or narrowed access to healthcare for residents of the state. Please see our previous article formore information on PHL 45-A here. Importantly, New York’s statute includes Managed Services Organizations (“MSOs”), even though they do not provide healthcare services themselves, as part of any healthcarerelated transaction subject to review.
 “I could do it in my pajamas. I didn’t have to drive anywhere,” explains Kelly. She accessed prescribed exercises through her personal portal and performed them with the assistance of video and motion tracking. “It is such a cool technology. You can really see if you’re doing things the right way.”
“I could do it in my pajamas. I didn’t have to drive anywhere,” explains Kelly. She accessed prescribed exercises through her personal portal and performed them with the assistance of video and motion tracking. “It is such a cool technology. You can really see if you’re doing things the right way.” Musculoskeletal treatments are also a top driver of rising health insurance costs.
Musculoskeletal treatments are also a top driver of rising health insurance costs. For patients suffering with a hernia, the pain, discomfort and disfiguration can be all too familiar. A hernia is essentially a hole in the abdominal or pelvic wall through which tissue can protrude, and while hernias are considered common, they can often be complex depending on the situation. However, regardless of complexity or severity, the team at the Hernia Center of Excellence at St. Joseph’s Health provides high quality care to all patients needing surgery due to a hernia.
For patients suffering with a hernia, the pain, discomfort and disfiguration can be all too familiar. A hernia is essentially a hole in the abdominal or pelvic wall through which tissue can protrude, and while hernias are considered common, they can often be complex depending on the situation. However, regardless of complexity or severity, the team at the Hernia Center of Excellence at St. Joseph’s Health provides high quality care to all patients needing surgery due to a hernia.


 repair has exploded in techniques and isbeing seen more as a subspecialty, rather than something that just anyone can take on,” she explained.
repair has exploded in techniques and isbeing seen more as a subspecialty, rather than something that just anyone can take on,” she explained. The team of surgeons at the Hernia Center of Excellence values ongoing communication with referring providers and the patients themselves, which helps achieve continuity of care extending through the time when patients return to seeing their primary care physicians.
The team of surgeons at the Hernia Center of Excellence values ongoing communication with referring providers and the patients themselves, which helps achieve continuity of care extending through the time when patients return to seeing their primary care physicians. “Ultimately, patients are anxious to get the help they need and get back home, and we want them to have a very good experience here,” said Dr. Belfield. “So, patients can expect a consistent experience in our office with good communication about what they can do to prepare for surgery, what’s going to happen during surgery and how they can recover best from surgery. The goal at our center is to provide the most durable and most appropriate option for each patient who comes through our doors.”
“Ultimately, patients are anxious to get the help they need and get back home, and we want them to have a very good experience here,” said Dr. Belfield. “So, patients can expect a consistent experience in our office with good communication about what they can do to prepare for surgery, what’s going to happen during surgery and how they can recover best from surgery. The goal at our center is to provide the most durable and most appropriate option for each patient who comes through our doors.” “Coming to work here, it’s really apparent from tip to tail that my other partners are tremendous. It’s rare that you get to be a part of a department where there’s not one person who doesn’t go above and beyond,” he said.
“Coming to work here, it’s really apparent from tip to tail that my other partners are tremendous. It’s rare that you get to be a part of a department where there’s not one person who doesn’t go above and beyond,” he said.


