By Elizabeth Landry

First Year Family Medicine Residents (L-R): Shramika Pokharel, MD, Urva Barot, MD, Roselyn Akukalia, MD, Nozima Akbarova, MD
2025 has proven to be a milestone year for Syracuse Community Health – it was the inaugural year for its new Family Medicine Residency Program, which offers a unique approach to family medicine training rooted in out-patient settings, community based care, and serving the needs of the most vulnerable patient populations. At the center of the program are the four residents leading the way in SCH’s new endeavor, which is led by Program Director Cristian Andrade, MD. Having already completed four years of undergraduate college and four years of medical school, these residents are training to become family medicine physicians who will offer comprehensive, continuous healthcare for people of all ages—infants, children, adults, and the elderly.
 Shramika Pokharel, MD, Urva Barot, MD, Nozima Akbarova, MD and Roselyn Akukalia, MD will each spend three years caring for diverse communities, rotating through SCH and Crouse Hospital in
Shramika Pokharel, MD, Urva Barot, MD, Nozima Akbarova, MD and Roselyn Akukalia, MD will each spend three years caring for diverse communities, rotating through SCH and Crouse Hospital in
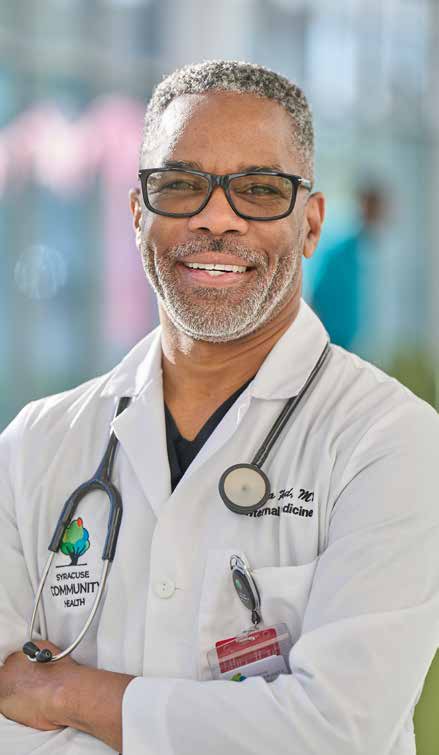
Syracuse, Rome Health in Rome, and Samaritan Medical Center in Watertown. At each location, they will learn from the physicians they train with as well as the patients they serve.
“Our new Family Medicine Residency Program is an exciting step forward for both medical education and community health,” said SCH CEO Ofrona Reid, MD. “By training residents in an underprivileged area, we are fostering innovative, compassionate care where it’s needed most. This program empowers future physicians to tackle health disparities head-on while strengthening the well-being of our entire community.”
While family medicine is one of the largest residency specialties in the United States, acceptance into family medicine residency programs is highly competitive. According to 2025 data from the National Resident Matching Program (NRMP), there are approximately 13,000 to 14,000 applicants per year for only about 5,500 to 5,800 available residency positions, resulting in an approximate match rate of 40-45%. By offering a new program that will actively train 12 family medicine residents over the next three years (and more anticipated in the years to come), SCH is creating more opportunities for residents while simultaneously helping to address the family medicine physician shortage in the Central New York community.
Dozienze Nwoke, MD, a family medicine physician from Long Island, came to SCH last year to help lead the program as the Assistant Program Director. “It’s very exciting, the fact that we’re able to produce highly trained physicians to go out into society and take care of our sick and needy,” he said. “The Syracuse population is a very underserved population, and it’s just a blessing to be part of a program that produces physicians that will go out there and help take care of the community.”
A Unique Blend of Innovation, Collaboration and Community
 As the first ambulatory teaching health center in the region, SCH’s Family Medicine Residency Program offers a unique, innovative, community-based model for training Central New York’s next generation of family physicians. Dr. Nwoke explained how the outpatient clinic setting sets the program apart and allows residents to gain a more wellrounded, community focused training.
As the first ambulatory teaching health center in the region, SCH’s Family Medicine Residency Program offers a unique, innovative, community-based model for training Central New York’s next generation of family physicians. Dr. Nwoke explained how the outpatient clinic setting sets the program apart and allows residents to gain a more wellrounded, community focused training.
“Because it’s an outpatient program, the basis is strictly in the community,” said Dr. Nwoke. “So that makes it totally different from anything else. Because we’re in a community-based program, we’re not connected directly to a hospital. Our residents do go into rotations at different places where they are exposed to inpatient care, but the main focus is outpatient medicine. We’re dealing with chronic issues, and our goal is to basically provide preventative care to the community, to teach them and educate them about different ways they can prevent different illnesses.”
Along with the community partnerships collaborating with health centers in Rome and Watertown, residents gain a big-picture view of healthcare in diverse settings and communities – something the residents themselves highly value.
“One of the aspects I value most about this program is its intentional design in exposing residents to both urban and rural healthcare settings,” said Dr. Barot. “Syracuse offers an urban patient population with complex social and cultural dynamics, while Rome and Watertown provide opportunities to care for rural communities facing unique challenges such as limited access to specialty care and resources. This dual exposure ensures we are trained to become well-rounded physicians— adaptable, culturally competent, and prepared to serve diverse populations in any setting.”
Dr. Akukalia offered similar sentiments – emphasizing how the program’s strong foundation of community-based, outpatient care most aligned with her own medical philosophy.

“What truly resonated with me was the program’s deep commitment to community engagement. The opportunity to build lasting relationships with patients, understand their unique social contexts, and contribute meaningfully to the health of underserved populations is exactly the kind of impact I aspire to make as a physician,” said Dr. Akukalia.
Commitment to Healing the Underserved
Perhaps the strongest draw to the Family Medicine Residency Program at SCH as expressed by residents is the opportunity to serve diverse and vulnerable patient populations while undergoing their training.
“Throughout my education and community work, I have been called to care for those who often go unheard, advocating for patients with limited resources. I see this residency as more than training; it’s an opportunity to grow into a physician I’ve always aspired to be: one who serves with compassion, humility, and dedication,” shared Dr. Pokharel.
Although Dr. Akbarova hasn’t yet rotated through the Watertown location, she shared how she has already learned so much from working with the underserved populations in Syracuse and Rome, and how her experiences are already shaping the way she approaches every patient interaction.
 “Working with such diverse populations has taught me to listen more deeply, to ask questions with respect, and to appreciate that every patient teaches me something new,” shared Dr. Akbarova. “No matter where they come from, my goal is always the same — to meet them where they are and help them feel seen, heard, and cared for… Every interaction, no matter how brief, is an opportunity to offer comfort and reassurance. Acting with responsibility, empathy, and respect helps patients feel supported through some of their most vulnerable moments.”
“Working with such diverse populations has taught me to listen more deeply, to ask questions with respect, and to appreciate that every patient teaches me something new,” shared Dr. Akbarova. “No matter where they come from, my goal is always the same — to meet them where they are and help them feel seen, heard, and cared for… Every interaction, no matter how brief, is an opportunity to offer comfort and reassurance. Acting with responsibility, empathy, and respect helps patients feel supported through some of their most vulnerable moments.”
Whole-Person, Patient-Centered Care
 Directly related to the outpatient setting in which residents learn to care for diverse, underserved populations is the program’s focus on forming physicians who care for the patient as a whole person and in every stage of life. Dr. Nwoke explained that, in accordance with SCH’s mission to provide high-quality care to every patient they serve, there are many questions residents learn to ask and consider when treating patients.
Directly related to the outpatient setting in which residents learn to care for diverse, underserved populations is the program’s focus on forming physicians who care for the patient as a whole person and in every stage of life. Dr. Nwoke explained that, in accordance with SCH’s mission to provide high-quality care to every patient they serve, there are many questions residents learn to ask and consider when treating patients.
“It’s not just about medication, it’s about the home. How’re things going at home? Are you able to eat well? Are you on some type of food assistance? Do you have shelter? Are you safe at home? Do you feel safe in your environment? We assist if they don’t have transportation. We treat the whole person, including their environment,” Dr. Nwoke said.
For Dr. Akbarova, her passion for treating patients by aiming to understand who they are as people and developing strong relationships with each individual is what initially drew her to family medicine.
“From the very beginning of my medical journey, I was drawn to the philosophy of family medicine — the opportunity to care for patients across all ages and life stages, to build relationships that go beyond a single visit, and to truly understand the stories behind each person’s health. I practiced as a family physician in my home country for a short time before coming to the United States, and that experience solidified my passion for the field. I found great meaning in continuity of care, in seeing how trust and consistency can transform not only outcomes, but also lives,” said Dr. Akbarova.
said Dr. Akbarova.
Dr. Pokharel identified an important connection between serving in the community setting and treating each patient as a unique individual throughout every stage of life. She said that’s how she feels she can make the most meaningful difference in patients’ lives.
“Training in a community setting allows me to be closely connected to patients’ everyday lives – to care for them not only when they are sick but also to promote wellness and prevent illness before it begins,” said Dr. Pokharel. “This environment reflects the true spirit of family medicine: being there for families through every stage of life, addressing diverse needs, and making a lasting impact through preventive care and health education.”
Investing in the Future of Healthcare
Just as the four residents are training to learn how to make the most positive, lasting impact on the lives of patients they serve, the Family Medicine Residency Program at SCH is also aimed at making a strong, positive impact on the future of healthcare itself in the Central New York region. The residents each spoke about the sense of honor they feel in being a part of the inaugural year and class of the program.
“There is a strong sense of responsibility and collaboration among those of us starting this journey together,” said Dr. Barot. “It’s inspiring to know that the work we do now will lay the foundation for future classes, and I am proud to be a part of that legacy from the very beginning.”
 Sharing how proud and grateful she is to be an SCH Family Medicine Resident, Dr. Akukalia said, “I see SCH as a beacon of hope for our community: a sanctuary where people find not only medical care, but also comfort, understanding and support for
Sharing how proud and grateful she is to be an SCH Family Medicine Resident, Dr. Akukalia said, “I see SCH as a beacon of hope for our community: a sanctuary where people find not only medical care, but also comfort, understanding and support for
their social and psychological needs. It’s a place of healing and refuge, where solutions are found and lives are uplifted.”
 Family Medicine Residency Program Coordinator Lori Chudyk shared her experience welcoming the residents into the program, and how she looks forward to the contributions they’ll go on to make as physicians in the future.
Family Medicine Residency Program Coordinator Lori Chudyk shared her experience welcoming the residents into the program, and how she looks forward to the contributions they’ll go on to make as physicians in the future.
“It has been truly wonderful to watch our four new residents grow during this first year of the Family Medicine Residency Program. From the interview process to helping them settle into a new city and witnessing their ‘first day of school,’ every step has been meaningful. I am so proud of each of them. My greatest joy will come in June 2028, when they complete their residency and fully transition into independent practicing physicians. What a journey it is to watch their transformation,” said Chudyk.
Perhaps Dr. Nwoke best summarized the overall goal of both SCH and the new Family Medicine Residency Program, as all involved continue to work to strengthen the safety net for the community for years to come: “I think it’s just about giving back to the community, to those that are less fortunate,” he said. “I think the best way we can help the community is by educating them and showing them we’re there. The best gift of life is to know you’ve helped someone – helped someone to live another day.”



 Planning strategy today requires holding steady while priorities continually shift. The answer to “What matters most?” often depends on where you sit within the health system. This brief overview blends both system- level and clinician perspectives.
Planning strategy today requires holding steady while priorities continually shift. The answer to “What matters most?” often depends on where you sit within the health system. This brief overview blends both system- level and clinician perspectives. Private equity (PE) investment in healthcare has grown quickly, reshaping how medical practices run day to day. For physicians and practice owners, selling to a PE firm is a complex decision. It can open doors for growth and support, but it also brings challenges. —offering strategic advantages and potential pitfalls. In New York State, strict regulatory constraints add another layer of complexity that need to be understood before moving forward.
Private equity (PE) investment in healthcare has grown quickly, reshaping how medical practices run day to day. For physicians and practice owners, selling to a PE firm is a complex decision. It can open doors for growth and support, but it also brings challenges. —offering strategic advantages and potential pitfalls. In New York State, strict regulatory constraints add another layer of complexity that need to be understood before moving forward.


 Auburn Community Hospital (ACH) is pleased to announce the appointment of Migdalia Bonilla-Martir, MD, FACOG, as Chief of Obstetrics and Gynecology.
Auburn Community Hospital (ACH) is pleased to announce the appointment of Migdalia Bonilla-Martir, MD, FACOG, as Chief of Obstetrics and Gynecology.