 After months of custom design and construction, Drakos Clinical Dynamics opened Drakos Pediatric Urgent Care on May 15, 2023, at the Clay Medical Center to address a critical shortage in accessible pediatric urgent care here in Central New York.
After months of custom design and construction, Drakos Clinical Dynamics opened Drakos Pediatric Urgent Care on May 15, 2023, at the Clay Medical Center to address a critical shortage in accessible pediatric urgent care here in Central New York.
“Our team is dedicated to innovating how healthcare services are provided so we can solve problems that have not yet been addressed,” says Drakos Founder and CEO

Heather Drake Bianchi. “Our team has a unique ability to address some of the community’s challenges because of the ways that we have made laboratory and medical services mobile.”
The Drakos Pediatric Urgent Care team includes experience from both pediatrics and emergency medicine, including physicians, physician assistants, nurse practitioners, registered nurses, radiology technicians, laboratory technicians, paramedics, and other healthcare professionals. They provide on-site radiology with portable and child-friendly x-rays, a comprehensive on-site laboratory, immediate on-site pain management and treatment for more severe conditions, and minor orthopedic care to provide fiberglass splints for fractures.
 Drake Bianchi was first inspired to start a pediatric urgent care when her two-month-old son, Greyson, tested positive for COVID in early 2022. The family was in Boston while Drake Bianchi worked on a film production with CineMedics, a Drakos subsidiary that provides medical testing and care on entertainment sets. Far from Greyson’s regular doctor, Drake Bianchi felt terrified for her baby. She reached out to a local pediatric urgent care.
Drake Bianchi was first inspired to start a pediatric urgent care when her two-month-old son, Greyson, tested positive for COVID in early 2022. The family was in Boston while Drake Bianchi worked on a film production with CineMedics, a Drakos subsidiary that provides medical testing and care on entertainment sets. Far from Greyson’s regular doctor, Drake Bianchi felt terrified for her baby. She reached out to a local pediatric urgent care.
“The pediatric urgent care was on the phone with me within 15 minutes,” she remembers. “They told me exactly where to hold the camera phone so they could see his breathing and evaluate his symptoms. They assured me that he was all right and what do to if his symptoms worsened. It was a huge relief and a lightbulb moment for me. I realized we didn’t have this resource in Central New York, but every parent and adult who cares for children needs it.”
Drake Bianchi is quick to point out that pediatric urgent care is not a replacement for primary care or emergency rooms. Instead, the Drakos team aims to be a responsible supplement and partner to them.

“Sometimes kids need to be seen at odd hours. As a parent, it sometimes feels like if your pediatrician’s office closes at 4:30 p.m., your child will get sick at 4:31 p.m.,” says Drake Bianchi. “We want to work with parents, guardians, primary care doctors, and emergency rooms to fill the gap so children who need care when their doctor’s office isn’t open, but whose conditions don’t require emergency care, can still receive the healthcare they need when they need it.”
Having a pediatric urgent care is also an important next step in strengthening Central New York’s healthcare infrastructure, especially as Micron builds its new semiconductor factory in Clay, where the pediatric urgent care is located.
“Central New York is anticipating significant population growth, so our healthcare infrastructure must grow as well,” says family medicine physician Dr. Zaki Badawy, MD, PC, who is also a Drakos Pediatric Urgent Care owner and the Medical Director. “Drakos Pediatric Urgent Care will be an essential new part of the healthcare safety net. We are excited to partner with primary care and emergency care providers to protect the health of our community and children.”
As Drakos was designing the pediatric urgent care, inclusion was one of their guiding values. The Drakos Pediatric Urgent Care team is committed to understanding and welcoming every patient. The new pediatric facility is designed to serve people with disabilities and special needs, ADA-compliant, and ready to serve patients who are non-mobile or home-bound.
To make children feel more comfortable during their visits, each examination room includes a one-of-a-kind mural with vibrant colors and imaginative designs. Working with local artist Mark Noble, the team set a goal of creating spaces that are inclusive, healing, and engaging for patients to help reduce patients’ nerves and ease stress around future visits.
Drakos also wanted to be attentive to treating children and supporting the entire family system. As a unique offering in Central New York, when children come into Drakos Pediatric Urgent Care for pediatric treatment, Drakos can provide wellness care to the pediatric patient’s parents or guardians at the same time as the pediatric patient’s appointment with include hydration, vitamins, and other fluid infusion services to help keep parents and other caregivers healthy.
“When a child is sick or hurt, it affects everyone who loves them. I understand that as a healthcare provider and a parent,” says Drake Bianchi. “Drakos Pediatric Urgent Care is here to support all children, their families, and our fellow clinicians who serve them. This is a thoughtfully designed inclusive environment that is comfortable for children, teens, and young adults up to the age of 26. It’s friendly and colorful in a way that welcomes all ages of growing up.”
The Drakos Pediatric Urgent Care offers convenient, compassionate, and expert care during after-school and evening hours from 2 p.m.-12 a.m., 7 days/week, with telehealth available 12 p.m.–12 a.m. It has options for in-office, virtual, and at-home care with easy scheduling, transparent pricing, and fast results that connect patients with the next step for the care they need.
Its offerings are designed with the understanding that parents—especially single parents and those living in low-income or rural areas—may not have easy access to transportation, healthcare facilities, or insurance coverage. Additionally, there are extremely limited options for pediatric urgent care in Central New York. Scheduling pediatric appointments when urgent care is needed and being seen in a timely manner are significant challenges in this community.
Established by a team of first responders and medical professionals, Drakos has experience delivering care in many different environments. Founded on the principle that quality healthcare should be delivered without walls or limits, Drakos addresses gaps in healthcare by bringing fast, accurate services to patients wherever they are. Drakos provides mobile laboratory and medical services for concierge medicine, senior citizens aging-in-place, and underserved populations who face barriers to accessing healthcare. The company is interested in partnering with and assisting other healthcare providers on a variety of projects, from revolutionizing the way care is delivered in Central New York to helping develop strategies to offering support for bottlenecks in testing and laboratory work. The company operates two custom-designed mobile labs and opened its first brick-and-mortar laboratory in East Syracuse last year.
For more information please see Drakos Dynamics – Biotech for Real Life!









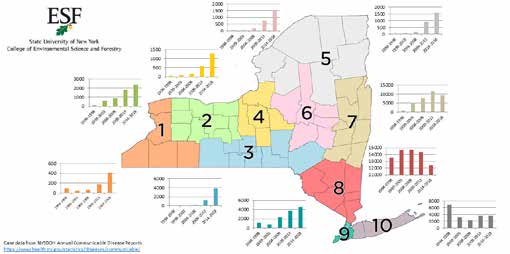
 Ticks can carry a variety of illnesses. The past few years, we are seeing new varieties of ticks with higher infection rates. The diseases they carry are often missed or mistaken for other illness and can quickly turn dangerous.
Ticks can carry a variety of illnesses. The past few years, we are seeing new varieties of ticks with higher infection rates. The diseases they carry are often missed or mistaken for other illness and can quickly turn dangerous.



 The mission of the New York Office of The Medical Inspector General (OMIG) includes enhancing the integrity of the Medicaid program by preventing and detecting fraudulent, abusive and wasteful practices within the Medicaid program. Pursuant to this mission, New York implemented compliance program requirements in 2009. Recently, amended regulations were adopted governing the implementation and operation of effective compliance programs for certain required Medicaid providers. These revised regulations include significant changes to the original regulations and will require affected Medicaid providers to review and revise their existing compliance programs. So, what steps should Medicaid providers take now to meet these new requirements?
The mission of the New York Office of The Medical Inspector General (OMIG) includes enhancing the integrity of the Medicaid program by preventing and detecting fraudulent, abusive and wasteful practices within the Medicaid program. Pursuant to this mission, New York implemented compliance program requirements in 2009. Recently, amended regulations were adopted governing the implementation and operation of effective compliance programs for certain required Medicaid providers. These revised regulations include significant changes to the original regulations and will require affected Medicaid providers to review and revise their existing compliance programs. So, what steps should Medicaid providers take now to meet these new requirements? For the past 30 years, Jenn Negley has worked in medical malpractice insurance, currently serving as Vice President of the National Healthcare Practice at Risk Strategies, a top, national independent specialty insurance brokerage firm. Along the way, she learned every facet of the business from managing accounts to production and brings that detailed expertise to her clients in New York state.
For the past 30 years, Jenn Negley has worked in medical malpractice insurance, currently serving as Vice President of the National Healthcare Practice at Risk Strategies, a top, national independent specialty insurance brokerage firm. Along the way, she learned every facet of the business from managing accounts to production and brings that detailed expertise to her clients in New York state. 









 Over the past several years, many in the U.S. have suffered poor mental health and suicide rates have remained steady. Working people tend to be affected by these issues at a high rate. A rise in remote employment leading to feelings of isolation as well as high-stress, fast-paced work environments are contributing factors to these patterns.
Over the past several years, many in the U.S. have suffered poor mental health and suicide rates have remained steady. Working people tend to be affected by these issues at a high rate. A rise in remote employment leading to feelings of isolation as well as high-stress, fast-paced work environments are contributing factors to these patterns.