Carthage Area Hospital
“We build almost everything except roads and bridges and infrastructure,” says owner and President Gary Crisalli, who’s been in the construction business for 45 years. “There’s no type of building construction work that we do not perform.”
From first job to first in the field
Crisalli says he was interested in medical construction early in his career and was encouraged by a previous business partner in the mid-1980s to bid on a remodel project at SUNY Upstate Medical University Hospital. G.M. Crisalli & Associates Inc. got the contract in 1990 and the project was completed in 1991. Crisalli successfully bid other projects at Upstate University Hospital and has done an increasing number of medical facility projects for all major hospitals and many private medical facilities throughout the company’s history.
New builds and renovations have unique considerations, from making sure existing services remain available to local, state and federal restrictions for various types of construction. Essential to successful healthcare-related projects is considering the special working conditions demanded of each worksite, such as the type, age and condition of the existing structure and current municipal services, knowing if the area will be kept operational by the medical group, and the availability and access during working hours. Are there quiet times and peak times during patient services for work crews to consider? Are all team players who will be affected by construction kept in communications to understand the impact on their ongoing operations?
“Less-experienced contractors may not know how to create and work within the restrictions of a protected environment, the impact of air filtration and quality air monitoring, and how to successfully manage those things for staff and patient safety and comfort,” Crisalli says. “Everything has to be kept very clean and dust-free, and you have to monitor airflow and air quality. You must be aware of all considerations involved in working in sterile environments. You must have good communication and control of the activities on the jobsite at all times, knowing who is there and what tools and materials are being delivered, installed and used throughout the construction of the project.”
Crisalli says when performing medical work of any kind, the scheduling process must be at the last third of the preconstruction process and extremely thorough — a must due to the long lead times on specialty materials and equipment needed for projects. Worked into that scheduling are staff and facility requirements during construction and all safety and code issues to be considered before, during and after construction completion.
“We like to have all stakeholders buy into the project schedule prior to project commencement to alleviate delays in the construction process,” Crisalli says.
Island Health Center in Ithaca, New York
Reputation for quality and integrity
“For the benefit of our clients, we try to bring our vast construction experience and knowledge to the project in order to be the best-trusted partner, liaison and friend before, during and after the project is finished,” Crisalli says. “Our reputation is based on our integrity, in the trust given to us by our many clients and in the accuracy in estimates, schedules, work quality and high level of professionalism. We take our responsibility as construction professionals very seriously. We believe our clients should rely on the professionals building the project and should not have to worry about the construction of a facility that they have hired our company to build for them.”
Crisalli says he employs 18 experienced project superintendents. He stated that one half of the company employees have been with G.M. Crisalli and Associates Inc. for up to 30 years. Crisalli feels very fortunate to have worked with Vice President Rocco “Rocky” Paone during that same time.
“Experienced and dedicated personnel, construction administration, construction procedures, practices and performance, at every milestone along the way, result in the highest-possible quality project,” Crisalli says. “At the end of the process, we want to see our clients satisfied and happy with every aspect of their new facility.”
Crisalli says the firm is always looking to integrate new systems to anticipate clients’ needs and ensure projects are turnkey operations at completion.
“Most of my people have been with us for quite a few years,” Crisalli says, “but we have a few new people, too, helping us do whatever we can to make us a better company. We have our own group of sub-contractors, offer competitive rates and have the capability to adapt and grow — like what was demanded of us working in a pandemic.”
One of those adaptations was the implementation of DocuSign to tame the contracting paper lion.
Work in progress at American Renal Associates Dialysis Center in Rome, New York
Client care is Job No. 1
Rocky handles the marketing and sales and performs the front-end of projects (the pre-construction functions formerly done under the umbrella of estimating).
“I also cold-call potential clients and follow up with clients whose projects are complete, as well as work to maintain relationships with a variety of professionals across a diverse field of disciplines,” Paone says.
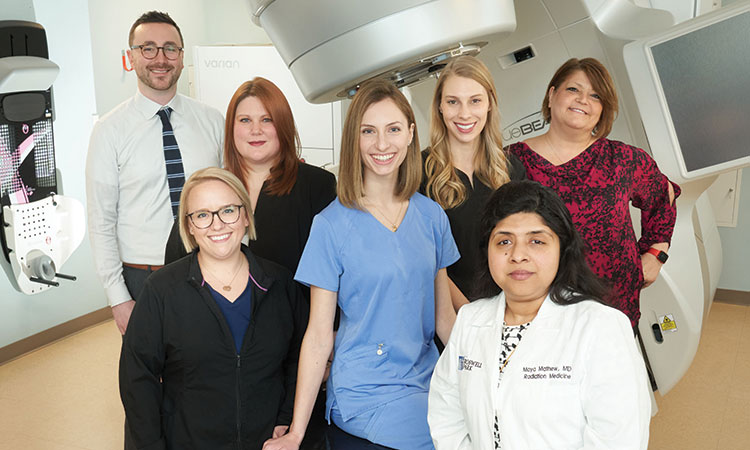
Medical construction requires a level of cleanliness more than most construction projects, Paone says, explaining that G.M. Crisalli and Associates Inc. understands the demands of working in something tantamount to a clean room environment.
“It’s not for everyone,” Paone says. “You can’t just take someone out of residential construction and tell them to go drywall an operating room. There are a specific list of additional dos and don’ts in the medical environment, and sometimes they impact patients’ lives and safety. We have to maintain stringent levels of quality control for these projects.”
In addition, the firm pays particular attention to the health of its own employees, making sure they are current with tuberculosis testing and additional health considerations, especially in the era of COVID-19.
“There are a lot of additional boxes we have to check to work in a medical setting of any kind,” Paone says.
And that medical savvy transfers to other projects requiring those heightened precautions, such as cleanliness and quality concerns.
“But we can build good, old-fashioned buildings, too,” Paone says.
University Hospital in Syracuse, New York
Project in progress
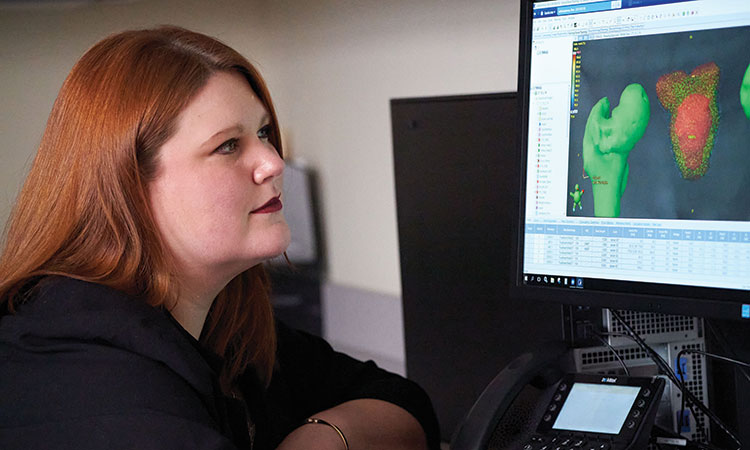
G.M. Crisalli is working on a tenant improvement fit-out for American Renal Associates Dialysis Center in Rome.
“We were competitively bidding the project and added G.M. Crisalli to the bid list based on the strength of their health portfolio and depth of knowledge exhibited by Rocco Paone,” says Marc Eagles of American Renal Management LLC, Project Management. “Construction projects are always challenging. This project was no different. G.M. Crisalli’s knowledge of the market, construction processes and subcontractor strength helped to make this a successful project.”
Money is a big motivator for clients, and medical clients are particularly cost-conscious and want to spend their money wisely.
“We work with clients to help them analyze budgets and look at what is really needed versus areas where savings can be safely realized,” Paone says. “If anti-static or anti-microbial flooring is called for, you really can’t compromise a lot there. We try to make clients aware of the trade-offs in these kinds of decisions. We’ve learned how to adapt to these details better than your average contractor and offer customers the pros and cons of every potential alternative and decision as they set up their budgets.
“We care about clients, we care what clients think about us, we care enough to tell the truth, even when the truth hurts,” Paone continues. “We’re all looking forward to a very rigorous 2021 season as COVID-19 waves its ugly head goodbye and we tackle the projects that were sidelined and those sprouting up as a result.”
“The medical field will grow because of the increasing aging population and new and improving technology,” Crisalli adds. “We plan to be at the forefront of that.”
“Without exception, every G.M. Crisalli employee involved with the project was professional, knowledgeable and easy to work with,” Eagles says. “I would recommend them on their construction acumen, professionalism and competitive pricing.”
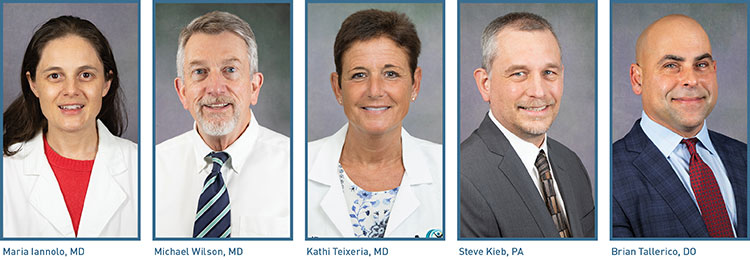
Medical project résumé
G.M. Crisalli’s project list includes extensive renovations, constructions and additions at SUNY Upstate Medical University, St. Joseph’s Hospital Health Center, Van Duyn Center for Rehabilitation & Nursing, Carthage Area Hospital, Nunn’s Home Medical Equipment, Crouse Hospital, Cayuga Medical Rehabilitation Center, Mohawk Glen and Health & Dental Services Center, among others.
Crisalli and Paone both say the Cayuga Medical Rehabilitation Center and Island Health & Fitness Center in Ithaca was one of their favorite projects. It included a two-and-a-half-year-long project consisting of design/project buildout of new tenant space and construction management services for a five-story health and fitness center with attached medical facility.
For more information, call 315-454-0000 or visit gmca.com.


























 “There has always been support 100% of the time for every emergency case, and it’s a huge responsibility for us to be able to provide the kind of care we provide to the community. It is a privileged role we have, and I feel fortunate that we are fully supported to take care of our patients and make sure they get the best treatment possible.”
“There has always been support 100% of the time for every emergency case, and it’s a huge responsibility for us to be able to provide the kind of care we provide to the community. It is a privileged role we have, and I feel fortunate that we are fully supported to take care of our patients and make sure they get the best treatment possible.”







