By Elizabeth Landry
Thursday, August 18, 2022
“The best care out there. Here.”

That’s the motto at Rome Health, an organization that is always focused on community and striving each day to provide patients with the best care possible. This commitment will now extend to the new Rome Health Medical Center, which opens this fall.
Located at 1500 N. James St. on the hospital’s main campus, the new Medical Center brings together primary care, surgical specialists, diagnostic testing and retail pharmacy services under one roof for coordinated, comprehensive, individualized patient care.
Careful Planning
Rome Health worked with King + King Architects and the Hayner Hoyt Corporation to design a building that intuitively offers ease of access and straightforward navigation right from the start of a patient’s experience. The new design also kept the provider experience in mind.
Providers from the hospital’s existing off-campus locations will move into the new 31,000-square-foot, two-story Medical Center over the next several months, as each office integrates with the center’s new electronic medical record. The facility includes 41 exam and procedure rooms with primary care, retail pharmacy and lab services on the ground floor. Additional primary care providers, general specialists and those specializing in breast and bariatric surgery will see patients on the second floor.
The proximity of adjacent services at the hospital, including medical imaging, cardiopulmonary services and cardiology, enhances accessibility for patients who may need multiple services but also face transportation difficulties.

Close Collaboration
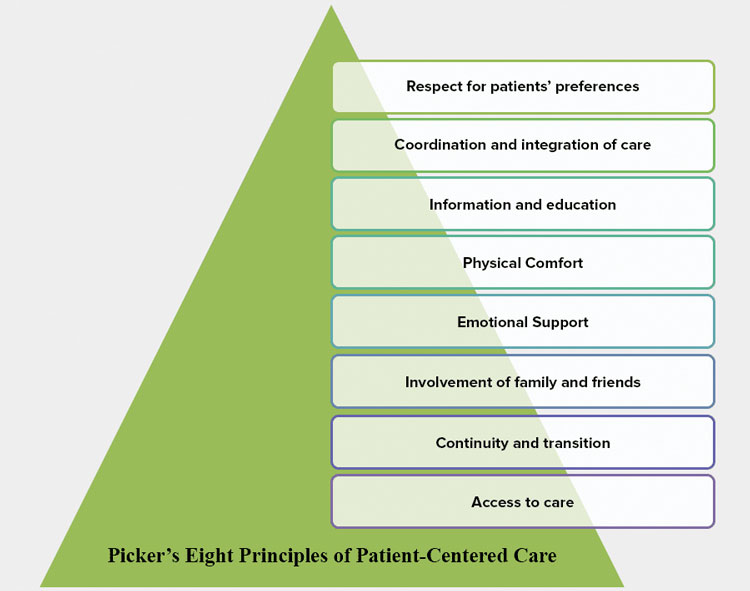
The Medical Center design supports providers and their care teams in delivering comprehensive care in an environment that is convenient and facilitates important healthcare discussions. Each floor is organized into separate pods, each one consisting of provider offices, a care team station and exam rooms. Allowing medical teams to quickly and easily collaborate enhances communication and supports coordinated patient care.
“This entire initiative really revolves around access to primary care and the coordination of care that comes out of that,” says Michael J. Attilio, MD, Vice President of Physician Practices at Rome Health. “This new space provides us with the opportunity to better integrate local primary care and specialty services, bring people together and have a much more collaborative and interactive environment. Providers can interact more frequently, which in primary care is very valuable. We take care of a very diverse population of individuals. Being able to simply walk next door and ask, ‘Hey, what do you think about this?’ helps us as clinicians to make better diagnoses and better decisions, which helps improve the quality of care our patients receive.”
Ryan Thompson, Chief Operating Officer, Rome Health Medical Center, says increasing ease of communication among providers and staff inherently comes with improved access to the community, as well.
“When we create an environment that supports the workflows of our physicians and nurse practitioners, it’s easier for them to just focus on our patients,” Thompson says. “Efficient workflows help us to increase capacity and offer greater access for our patients.”

A New Electronic Health Record System
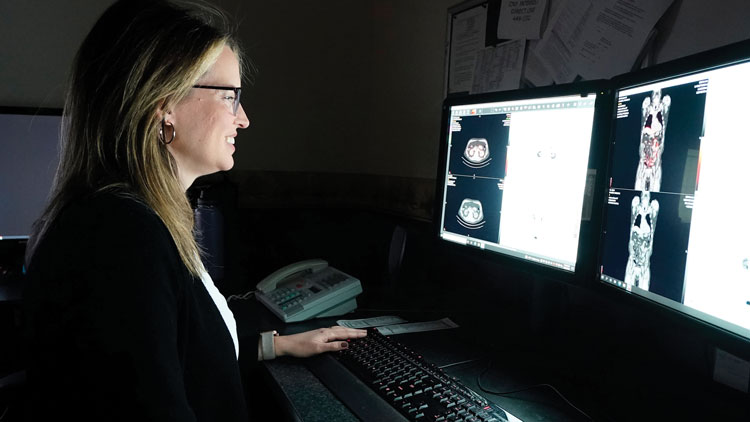
Another major component of the new Rome Health Medical Center is an integrated ambulatory electronic health record that will replace the stand-alone systems used by its affiliated primary care, prenatal care services and specialty practices. The new system will allow clinicians to access all of a patient’s medical information within the Rome Health system, regardless of where they were treated. Moving to a single platform also provides patients access to a portal where they can securely obtain their personal health information.
The new system will also help reduce unnecessary over testing and repeat medical testing.
“The integrated health record is going to assist physicians with communication amongst each other so we’re not duplicating efforts and care for patients,” says Chief Medical Officer Cristian Andrade, MD. “There’s going to be better access to those records when patients are admitted to the hospital, reducing the cost and improving efficiency and care for patients. From a population health standpoint, the electronic health record integration also helps with standardizing care for chronic conditions with evidence-based medicine.”
As a whole, the new Medical Center and its integrated systems will create a connected healthcare experience that benefits both patients and providers — a tool to help improve the lives and health of people in Rome and its surrounding communities.
As the official opening of the medical center approaches, the healthcare team at Rome Health will grow alongside the patient population they serve. But no matter where the care is being offered, serving patients with the best, coordinated and comprehensive care will always be at the heart of Rome Health.
“The really important thing I want everyone to reflect on as we move into this space is that at the end of the day, it’s really not about the space, if you think about it. It’s about the people in that space, our people taking care of the people who depend upon us for their care,” Dr. Attilio says. “We want to provide a comfortable, welcoming, high-quality environment for the patients we serve and the healthcare professionals who deliver that care.”
Visit romehospital.org to learn more.








 Andrew Wickline, MD
Andrew Wickline, MD Siobhan Fitzgerald, RN, BSN, Nurse Administrator
Siobhan Fitzgerald, RN, BSN, Nurse Administrator