By: Elizabeth Landry
 From breast cancer surgery, hernia repairs and laparoscopic surgery, to endocrine surgery, ulcer care, bariatric surgery and more, the Crouse Medical Practice General Surgery team offers a wide array of surgical procedures to help patients return to health and continue enjoying their lives. The team of 12 physicians brings a vast depth of knowledge and experience that combine to create a supportive practice that consistently focuses on patient-centered care. This patient-focused philosophy is built upon collaboration with the team, including primary care providers, as Clinton Ingersol, MD, Hillary McMullin, MD, Benjamin Sadowitz, MD, FACS and Angelina Schwartz, MD each explained in their own words.
From breast cancer surgery, hernia repairs and laparoscopic surgery, to endocrine surgery, ulcer care, bariatric surgery and more, the Crouse Medical Practice General Surgery team offers a wide array of surgical procedures to help patients return to health and continue enjoying their lives. The team of 12 physicians brings a vast depth of knowledge and experience that combine to create a supportive practice that consistently focuses on patient-centered care. This patient-focused philosophy is built upon collaboration with the team, including primary care providers, as Clinton Ingersol, MD, Hillary McMullin, MD, Benjamin Sadowitz, MD, FACS and Angelina Schwartz, MD each explained in their own words.
“To me, the philosophy of our group revolves around patient-centered care and collaboration. It’s just been a very supportive environment and a supportive team to walk
into, and I think that really benefits patients,” said Dr. Ingersol, a newer provider within the team who’s been with Crouse for almost two years.
Dr. Sadowitz has been working at Crouse for 10 years. He stated that one of the major reasons he chooses to practice at Crouse is the healthcare organization’s focus on patient satisfaction, making sure that each patient feels supported and valued.
“Patients want to feel like they’re being treated as human beings, and I think Crouse does an exemplary job of that from start to finish. You’ll find that patients are very highly complementary in that respect, and that’s one of the reasons I want to work at Crouse – patients feel that they’re part of a broader family and that they’re going to be taken care of in the same way we take care of our friends or family members,” explained Dr. Sadowitz.
Collaborative Support for Each Other and Patients Alike
Both Dr. McMullin and Dr. Schwartz have been practicing at Crouse for about a year, and they each expressed similar goals of building relationships with patients early on, to help them feel as comfortable as possible throughout the surgery process. Dr. McMullin was inducted into the Gold Humanism Honor Society while attending the University of South Florida, which focuses on managing the patient as a whole and not seeing patients as a series of medical conditions, a philosophy she carries over into her practice at Crouse.
“I find that when patients come into the office, they’re often nervous and scared to be seeing a surgeon at all,” Dr. McMullin said. “They know they’re going to have to be asleep for some portion of their care, and that gives them anxiety. If a surgeon can establish a rapport with a patient and develop a trust in the office before surgery, patients end up doing much better. I bring that philosophy to every patient I see. I think it’s really important to meet people where they are and to put them at ease from a social and emotional standpoint before we even get into the medical aspect of their care.”
 Similarly, for Dr. Schwartz, her approach to patient care is focused on open communication and reaching decisions together as a team.
Similarly, for Dr. Schwartz, her approach to patient care is focused on open communication and reaching decisions together as a team.
“Whenever a patient comes to see me in the office, we try to have a conversation essentially about what it is that should happen, and what the recommendations are. Ultimately, it’s a decision that I like to think we come together as a team to decide – both patient and doctor together deciding what’s best for that individual person,” explained Dr. Schwartz, adding that the team aims to make the referral and scheduling process as efficient and convenient as possible for patients.
 Open lines of communication and support apply not only to patient care, but also to how the team works together to provide optimal healthcare for patients, as Dr. Schwartz emphasized.
Open lines of communication and support apply not only to patient care, but also to how the team works together to provide optimal healthcare for patients, as Dr. Schwartz emphasized.
“We have a very collaborative group of surgeons here, and all of us openly communicate with each other. Oftentimes we’re working together very closely in discussion of patient cases. We just really like to work together amongst ourselves and also amongst our colleagues within the hospital and even outside the hospital and in the local community. We try to work pretty closely with everyone around us,” she said.
 Dr. Ingersol echoed these ideas, highlighting the streamlined communication process within the Crouse healthcare network specifically. “It’s great for patients when everyone is on the same page and communicating in a multidisciplinary fashion. Especially within the Crouse network, it’s so easy to communicate with our primary care colleagues. We can send direct messages to each other to coordinate patient care and ask questions. Our office staff does a great job of coordinating referrals from primary care offices, making sure that patients are seen according to urgency, and making sure things are followed up on and communicated properly,” he explained.
Dr. Ingersol echoed these ideas, highlighting the streamlined communication process within the Crouse healthcare network specifically. “It’s great for patients when everyone is on the same page and communicating in a multidisciplinary fashion. Especially within the Crouse network, it’s so easy to communicate with our primary care colleagues. We can send direct messages to each other to coordinate patient care and ask questions. Our office staff does a great job of coordinating referrals from primary care offices, making sure that patients are seen according to urgency, and making sure things are followed up on and communicated properly,” he explained.
Collective Experience Paired with a Fresh Perspective
Directly related to the high level of collaboration among the Crouse Medical Practice General Surgery team is the way the providers lean on each other’s diverse experience and unique perspectives. Dr. McMullin highlighted the mix of well established surgeons with younger providers offers immense benefits for patients.
“We have a wide range of practitioners at Crouse General Surgery. Some of our more senior partners have been in practice my entire life. Then we have a few surgeons who have only been practicing for one or two years. That range of experience really offers a lot of benefits to patients because our more senior partners obviously have a great deal of experience – they’ve seen many different conditions and anomalies, whereas the younger practitioners trained in an era where technology is more common and prevalent – for example, we received robotics training in residency,” said Dr. McMullin. “Our senior partners have been very gracious about including us in their patient care. They really enjoy having us come along and assist with interesting or challenging cases. They also elicit our feedback on some of the cases they’ve managed to see what we would do, with our fresh perspectives.”
Dr. Ingersol, who specializes in endocrine surgery, shared how working with the more experienced surgeons in the group has led to an exchange of techniques and strategies that enhances patient care, especially when it comes to making decisions on complex, high-risk cases.
 “Our senior partner, Dr. Schu, has been great to work with, has been a very willing mentor, and we frequently do cases together. There’s been a lot of exchange of ideas and techniques because I bring in certain expertise, knowledge and biases and he has this wealth of experience and way of doing things. Having all of that at our disposal to decide what is in the best interest of patients is really valuable,” Dr. Ingersol explained. “Any time I have a case that I anticipate being difficult or may run into something I wasn’t anticipating preoperatively, there’s always someone who’s more than willing to come in and take a look or join me if needed. That’s one of the advantages of a big group that has so much experience.”
“Our senior partner, Dr. Schu, has been great to work with, has been a very willing mentor, and we frequently do cases together. There’s been a lot of exchange of ideas and techniques because I bring in certain expertise, knowledge and biases and he has this wealth of experience and way of doing things. Having all of that at our disposal to decide what is in the best interest of patients is really valuable,” Dr. Ingersol explained. “Any time I have a case that I anticipate being difficult or may run into something I wasn’t anticipating preoperatively, there’s always someone who’s more than willing to come in and take a look or join me if needed. That’s one of the advantages of a big group that has so much experience.”
Advanced Robotics and Innovative Surgical Techniques
Perhaps one of the most important ways the Crouse Medical Practice General Surgery team sets itself apart from other surgery programs is its focus on advanced surgical procedures, especially robotics, as Dr. Sadowitz explained. He shared how the Crouse administration provided crucial support to surgeons during the time when robotics was starting to take off, and how Crouse’s robotics program today is the largest and most experienced in the region.
“The administrators asked us surgeons, ‘Do you think this is the future?’ and ‘Do you think this is something that we should invest  in?’ To their credit, once we told them robotics really is going to be the future for many service lines in surgery, they jumped in with both feet. They made an investment of both time and money because they saw how robotics was going to be better for patients, and they trusted our judgment,” said Dr. Sadowitz, adding that the general surgery team at Crouse now has 11 robots at its disposal, including the DV5, one of the newest systems, as well as an SP robot, Xi systems and a smaller X system.
in?’ To their credit, once we told them robotics really is going to be the future for many service lines in surgery, they jumped in with both feet. They made an investment of both time and money because they saw how robotics was going to be better for patients, and they trusted our judgment,” said Dr. Sadowitz, adding that the general surgery team at Crouse now has 11 robots at its disposal, including the DV5, one of the newest systems, as well as an SP robot, Xi systems and a smaller X system.
While all the surgeons on the Crouse General Surgery team are familiar with and comfortable using robotics for surgery, the younger members of the team have the added advantage of having experienced robotic technology in their residencies.
“Dr. McMullin and I happened to go to a residency that is more advanced in its surgical robotic training than most other programs. We came out of training having a really good grasp on robotic techniques. I think I graduated with more than 100 cases that I had performed on the robot already, which is fantastic,” shared Dr. Schwartz.
In addition to robotics, the Crouse General Surgery team is exploring other exciting advancements in surgical treatments. In the endocrine surgery space, Dr. Ingersol discussed a new treatment of thyroid nodules that’s on the horizon.
 “In thyroid care, one thing that we’re starting to look into is a new technology called RFA, or radiofrequency ablation,” Dr. Ingersol said. “We’re not in an active phase yet, but it’s something that’s in the near future across the country and becoming a popular modality of treating thyroid nodules.”
“In thyroid care, one thing that we’re starting to look into is a new technology called RFA, or radiofrequency ablation,” Dr. Ingersol said. “We’re not in an active phase yet, but it’s something that’s in the near future across the country and becoming a popular modality of treating thyroid nodules.”
Dr. McMullin also highlighted an exciting new application of laparoscopic surgery aimed at treating patients with bile duct stones. “This type of laparoscopic exploration is something that’s not offered in very many places, and can be really valuable for patients,” she said.
Preparing for the Surgical Needs of Tomorrow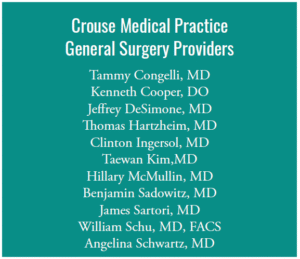 With an administration that invests in cutting edge technologies, and a team of forward-looking surgeons always interested in the latest up-and-coming treatments for patients, it seems the Crouse Medical Practice General Surgery team is well-prepared for the evolving needs of patients and will continue to thrive.
With an administration that invests in cutting edge technologies, and a team of forward-looking surgeons always interested in the latest up-and-coming treatments for patients, it seems the Crouse Medical Practice General Surgery team is well-prepared for the evolving needs of patients and will continue to thrive.
 “The future is very bright for Crouse in terms of overall surgery, with many great surgeons and a lot of advanced technology. The administration has made it a priority to make sure we stay technologically ahead of the game, so that’s a big piece of it,” said Dr. Sadowitz. “Crouse has always had the right mindset of ‘patients come first’ from the top down. The hospital always aims to keep very talented people in the hospital doing cases, so that not only are the patients highly satisfied, but the surgeons are, too. It’s a unique mix you really don’t find in many places, and it’s a hard balance to maintain, but Crouse has always excelled at doing just that, and as long as we keep that focus, I think it will continue into the future.”
“The future is very bright for Crouse in terms of overall surgery, with many great surgeons and a lot of advanced technology. The administration has made it a priority to make sure we stay technologically ahead of the game, so that’s a big piece of it,” said Dr. Sadowitz. “Crouse has always had the right mindset of ‘patients come first’ from the top down. The hospital always aims to keep very talented people in the hospital doing cases, so that not only are the patients highly satisfied, but the surgeons are, too. It’s a unique mix you really don’t find in many places, and it’s a hard balance to maintain, but Crouse has always excelled at doing just that, and as long as we keep that focus, I think it will continue into the future.”
For the younger providers who will carry the practice on into the next generation, this sentiment is certainly holding true.
“I plan on being here for a long time. It’s a great place to practice,” said Dr. McMullin. “The patient population is fantastic. The healthcare professionals are fantastic. I don’t plan on being anywhere else.”


 Driving across the western side of the Adirondacks, I made my way to a board strategy session held at The Beeches Manor in Rome, NY—a vibrant place in years past, once known for hosting weddings and proms. I knew it had recently been acquired by Nascentia Health, and I was delighted to see a beautifully restored restaurant and conference center, along with signs of new construction. The site is being transformed into a wellness-focused campus that will eventually offer a variety of assisted living levels and home-like services promoting active aging.
Driving across the western side of the Adirondacks, I made my way to a board strategy session held at The Beeches Manor in Rome, NY—a vibrant place in years past, once known for hosting weddings and proms. I knew it had recently been acquired by Nascentia Health, and I was delighted to see a beautifully restored restaurant and conference center, along with signs of new construction. The site is being transformed into a wellness-focused campus that will eventually offer a variety of assisted living levels and home-like services promoting active aging. When I asked Andrea what guidance she gives clinicians whose patients are aging and asking questions about the future, she emphasized the importance of early planning. Her advice: choose the best housing option early so you can age in place.
When I asked Andrea what guidance she gives clinicians whose patients are aging and asking questions about the future, she emphasized the importance of early planning. Her advice: choose the best housing option early so you can age in place. Technology plays a major role in the healthcare sector’s ability to store and handle private patient data. This has improved the efficiency of healthcare delivery, but it has also increased the susceptibility of healthcare providers to cyberattacks. The healthcare industry has witnessed a rise in cyber threats, including ransomware attacks, phishing scams, and data breaches. As a result, medical professionals need to take precautions against online threats to both themselves and their patients. A comprehensive Cyber insurance policy is one way to accomplish this.
Technology plays a major role in the healthcare sector’s ability to store and handle private patient data. This has improved the efficiency of healthcare delivery, but it has also increased the susceptibility of healthcare providers to cyberattacks. The healthcare industry has witnessed a rise in cyber threats, including ransomware attacks, phishing scams, and data breaches. As a result, medical professionals need to take precautions against online threats to both themselves and their patients. A comprehensive Cyber insurance policy is one way to accomplish this.

 Almost two years ago, New York enacted PHL Article 45 A, which took effect on August 31, 2023. One of the intents behind this law was flagging large business consolidation in the healthcare field, potentially allowing New York’s Department of Health to regulate the increased transaction prices, reduced competition, or narrowed access to healthcare for residents of the state. Please see our previous article formore information on PHL 45-A here. Importantly, New York’s statute includes Managed Services Organizations (“MSOs”), even though they do not provide healthcare services themselves, as part of any healthcarerelated transaction subject to review.
Almost two years ago, New York enacted PHL Article 45 A, which took effect on August 31, 2023. One of the intents behind this law was flagging large business consolidation in the healthcare field, potentially allowing New York’s Department of Health to regulate the increased transaction prices, reduced competition, or narrowed access to healthcare for residents of the state. Please see our previous article formore information on PHL 45-A here. Importantly, New York’s statute includes Managed Services Organizations (“MSOs”), even though they do not provide healthcare services themselves, as part of any healthcarerelated transaction subject to review.
 “I could do it in my pajamas. I didn’t have to drive anywhere,” explains Kelly. She accessed prescribed exercises through her personal portal and performed them with the assistance of video and motion tracking. “It is such a cool technology. You can really see if you’re doing things the right way.”
“I could do it in my pajamas. I didn’t have to drive anywhere,” explains Kelly. She accessed prescribed exercises through her personal portal and performed them with the assistance of video and motion tracking. “It is such a cool technology. You can really see if you’re doing things the right way.” Musculoskeletal treatments are also a top driver of rising health insurance costs.
Musculoskeletal treatments are also a top driver of rising health insurance costs.